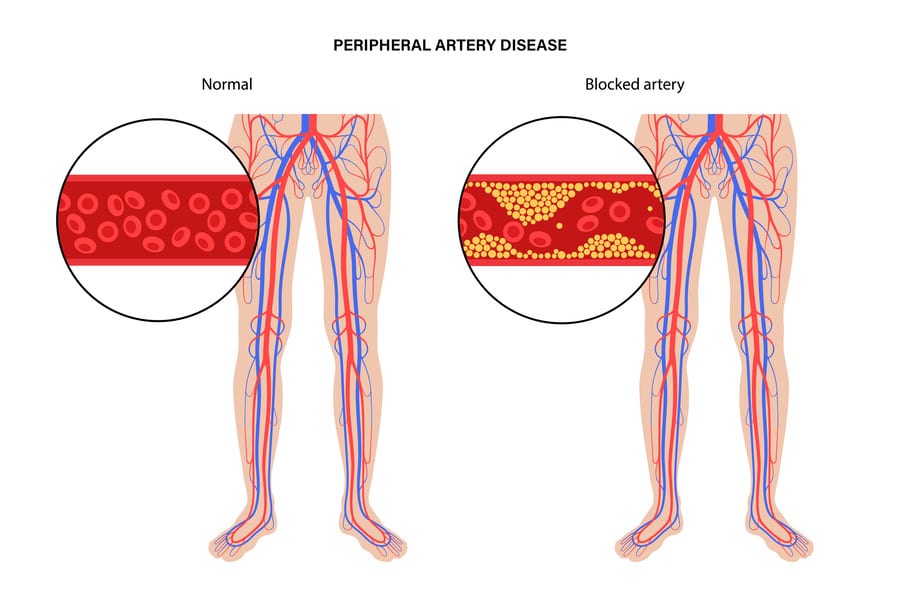
Peripheral Artery Disease (PAD) is a common circulatory condition characterized by narrowed arteries, reducing blood flow to the limbs, particularly the legs. PAD is primarily a result of atherosclerosis, a process wherein fatty deposits (plaques) accumulate on the arterial walls, narrowing and hardening the arteries.
Overview
PAD primarily affects the legs, but it can also involve the arteries that supply blood to the arms, head, and stomach. It’s an underdiagnosed condition, often mistaken for other health issues. Untreated PAD increases the risk of heart attack, stroke, and limb amputation due to critical limb ischemia (severe lack of blood flow).
Symptoms
PAD may be asymptomatic or present with various symptoms, including:
- Claudication: Pain or discomfort in the leg muscles (calves, thighs, or buttocks) while walking, which usually resolves at rest.
- Leg Weakness or Numbness: Reduced blood flow can lead to a feeling of weakness or numbness in the legs.
- Coldness in the Lower Leg or Foot: One leg may feel noticeably colder than the other due to decreased blood flow.
- Sores on the Toes, Feet, or Legs: Slow-healing or non-healing sores on the lower extremities can indicate PAD.
- Change in Leg Color: Reduced blood flow can lead to color changes in the skin of the legs.
- Hair Loss or Slower Hair Growth: Reduced blood flow can affect hair growth on the legs.
- Shiny Skin: The skin on the legs may appear shiny due to reduced blood supply.
- Weak Pulse in the Legs or Feet: Absent or weak pulses in the legs or feet can indicate PAD.
- Erectile Dysfunction: In men, PAD can sometimes cause erectile dysfunction.
Causes
The primary cause of PAD is atherosclerosis. Other factors contributing to PAD include:
- Blood Clots- In some cases, PAD can be caused by blood clots that block blood flow in the arteries. These clots can form anywhere in the body and travel to the peripheral arteries, where they can lodge and reduce or block blood flow. Conditions that increase the risk of blood clot formation include atrial fibrillation, deep vein thrombosis (DVT), and certain clotting disorders.
- Vasculitis- Vasculitis is an inflammation of the blood vessels that can cause narrowing or blockage of the arteries. It’s a less common cause of PAD and can occur as a result of autoimmune diseases like rheumatoid arthritis or systemic lupus erythematosus.
- Limb Injury- Trauma or injury to the limbs can damage the arteries and reduce blood flow. This may include accidents, falls, or surgeries that damage the blood vessels.
Risk Factors
Factors increasing the risk of PAD include:
- Age: PAD is more common in individuals over 50.
- Smoking: Smoking is a significant risk factor for PAD.
- Diabetes: Diabetes increases the risk of atherosclerosis.
- High Blood Pressure: Hypertension can contribute to atherosclerosis.
- High Cholesterol: Elevated cholesterol levels can lead to plaque formation.
- Obesity: Excess weight increases the risk of PAD.
- Physical Inactivity: Lack of exercise contributes to PAD risk.
- Family History: Genetic factors can increase PAD risk.
How to Avoid PAD
To reduce the risk of PAD:
- Quit Smoking: If you smoke, quit. This is the most crucial step to prevent PAD.
- Control Blood Sugar: If you have diabetes, manage your blood sugar levels.
- Lower Cholesterol: Eat a heart-healthy diet and consider cholesterol-lowering medications.
- Exercise: Engage in regular physical activity, such as walking.
- Maintain a Healthy Weight: Lose weight if you’re overweight.
When to See the Doctor
Consult your healthcare provider if you have leg pain when walking, non-healing sores, or any other PAD symptoms. Early diagnosis is vital to prevent complications.
Treatment
Treatment for PAD focuses on reducing symptoms, improving limb function, and preventing complications. Options include:
- Lifestyle Modifications: Quit smoking, exercise, eat healthily, and manage chronic conditions.
- Medications: Drugs to lower cholesterol, manage blood pressure, or prevent blood clots may be prescribed.
- Angioplasty or Stenting: These procedures can open narrowed or blocked arteries.
- Bypass Surgery: A graft can reroute blood flow around a blocked artery.
- Thrombolytic Therapy: Medications can dissolve blood clots.
In conclusion, Peripheral Artery Disease (PAD) is a serious condition that requires timely diagnosis and management. Understanding the risk factors, adopting a healthy lifestyle, and seeking early medical intervention are crucial for preventing complications and maintaining overall vascular health.