Dilated cardiomyopathy, often shortened to DCM, represents a significant segment of heart disorders. This disease affects thousands globally, bringing to the fore the critical nature of understanding, diagnosing, and managing it effectively. This article delves deep into the nuances of DCM, shedding light on its every facet.
Definition
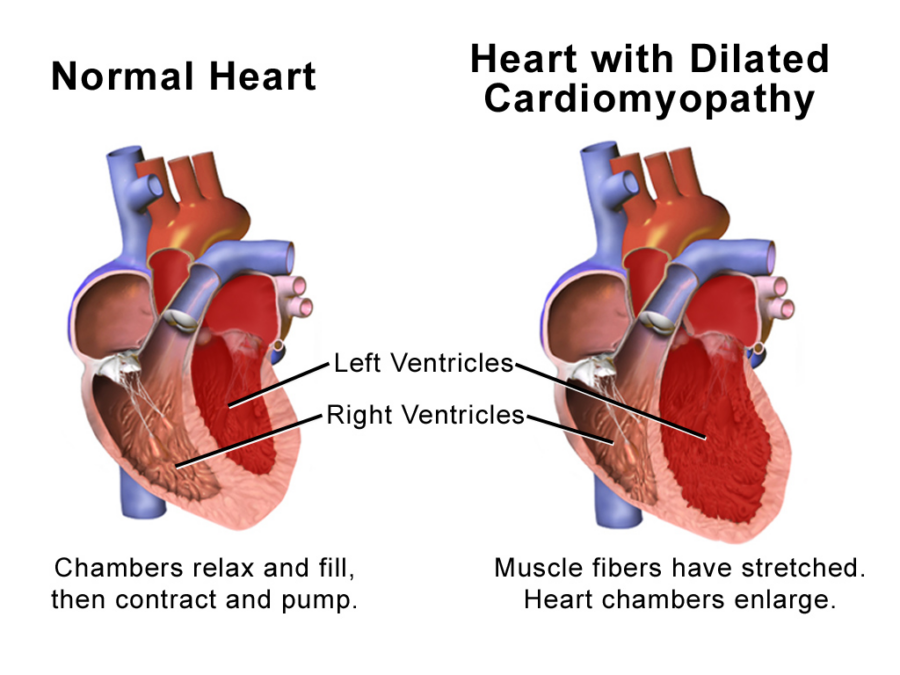
Dilated Cardiomyopathy (DCM) is a disease of the heart muscle where it becomes enlarged and can’t pump blood efficiently. The condition mostly affects the heart’s left ventricle, which is the primary pumping chamber.
Overview
The enlargement of the heart in DCM usually starts in the left ventricle. As the disease progresses, heart performance deteriorates, potentially leading to heart failure and associated complications. It’s a condition that can affect individuals across different age groups and has various causes.
Symptoms
The symptoms of DCM can range from none to severe, often depending on the stage of the disease. Some of the most common symptoms include:
- Fatigue
- Shortness of breath (even during rest or especially when lying down)
- Swelling in the ankles, feet, and legs
- Rapid or irregular heartbeats
- Lightheadedness or fainting
- Chest pain or pressure
- Reduced ability to exercise
Causes
While DCM can sometimes be idiopathic (meaning its cause is unknown), several factors can lead to its development:
- Genetic Predisposition: DCM can run in families, pointing to a potential genetic connection.
- Viral Infections: Some viruses can affect the heart and trigger DCM.
- Alcohol and Drugs: Chronic excessive alcohol consumption or cocaine use can weaken the heart muscle.
- Toxins: Exposure to certain toxins, including some chemotherapy drugs, can lead to DCM.
- Other Conditions: Uncontrolled hypertension, thyroid disorders, or diabetes can contribute to its onset.
Risk Factors
Understanding risk factors is crucial. Some of the most common ones include:
- Family History: Those with a family member with DCM are at a higher risk.
- Alcoholism: Chronic excessive drinking.
- High Blood Pressure: Chronic uncontrolled blood pressure.
- Certain Infections: Especially viral infections that affect the heart.
Avoiding DCM
While it might not be possible to avoid DCM entirely, especially when genetics are involved, there are steps one can take:
- Regular Check-ups: Frequent medical check-ups can catch potential heart problems early.
- Healthy Lifestyle: Balanced diet, exercise, limited alcohol consumption, and avoiding illicit drugs.
- Manage Chronic Conditions: Ensure conditions like diabetes or hypertension are well-managed.
- Avoid Infections: Regular hand washing, vaccines, and avoiding sick individuals can reduce the risk of viral infections.
When to See the Doctor
Immediate medical attention or a consultation with a cardiologist is crucial when:
- Experiencing persistent chest pain.
- Feeling fatigued or short of breath more often.
- Noticing a rapid, fluttering, or irregular heartbeat.
- Experiencing frequent fainting spells.
More Helpful Information
- Diagnostic Tests: These might include blood tests, chest X-rays, echocardiograms, MRI, CT scans, and more.
- Treatment: Depending on the severity, treatments can range from medications (like ACE inhibitors or beta-blockers) to devices (like pacemakers or defibrillators) and, in severe cases, heart transplants.
- Prognosis: While DCM is a serious condition, many individuals live long, healthy lives with proper management.
- Support Groups: Living with DCM can be challenging, but support groups, both online and offline, can provide invaluable resources and emotional support.
Potential Complications
DCM’s reduced heart function can lead to numerous complications:
- Heart Failure: The most common complication, where the heart can’t pump enough blood to meet the body’s needs.
- Heart Arrhythmias: Abnormal heart rhythms can become life-threatening if not managed.
- Thromboembolism: The inefficient pumping can lead to blood clot formation. If these clots leave the heart, they can block blood flow elsewhere in the body.
- Cardiogenic Shock: A severe form where the heart can’t supply enough blood to the body, it’s life-threatening.
The Role of Genetics in DCM
Recent research indicates a significant genetic component in DCM. Specific mutations in the genes encoding cytoskeletal, sarcomere, and nuclear envelope proteins have been identified. Genetic testing and counseling can be valuable, especially if DCM runs in families.
Current Research and Advances
Modern medicine is continually evolving, and DCM is no exception:
- Gene Therapies: Targeting the genetic causes of DCM.
- Stem Cell Research: Investigating if damaged heart muscle can be regenerated.
- Advanced Imaging Techniques: Providing more in-depth insights into the heart’s structure and function, enabling earlier detection.
Lifestyle and DCM
Beyond medical interventions, lifestyle plays a crucial role in managing DCM:
- Diet: A low-salt diet can prevent fluid accumulation, reducing the strain on the heart.
- Exercise: While intense physical activity might be harmful, light to moderate exercise, under medical supervision, can be beneficial.
- Monitoring Fluid Intake: To prevent fluid overload, which can exacerbate heart failure symptoms.
- Avoiding Alcohol and Tobacco: Both can worsen the condition and interfere with medications.
Support for Patients with DCM
Dealing with DCM can be emotionally challenging. Thus, psychological and social support is essential:
- Counseling: Discussing feelings and coping mechanisms with a professional can be therapeutic.
- Patient Networks: Connecting with others who have DCM can provide emotional support and practical advice.
- Educational Resources: Numerous organizations offer educational materials, workshops, and seminars on DCM.
Understanding Dilated Cardiomyopathy is vital, not just for those diagnosed but for the broader public. Awareness and knowledge can lead to early detection, more effective treatments, and ultimately, better health outcomes. As with many medical conditions, the key lies in education, early intervention, and effective management.