Wolff-Parkinson-White (WPW) syndrome is a congenital heart condition characterized by the presence of an extra electrical pathway in the heart. This additional pathway can lead to rapid heartbeats, known as tachycardia. The syndrome is named after the three physicians who first described it in the early 20th century.
Overview
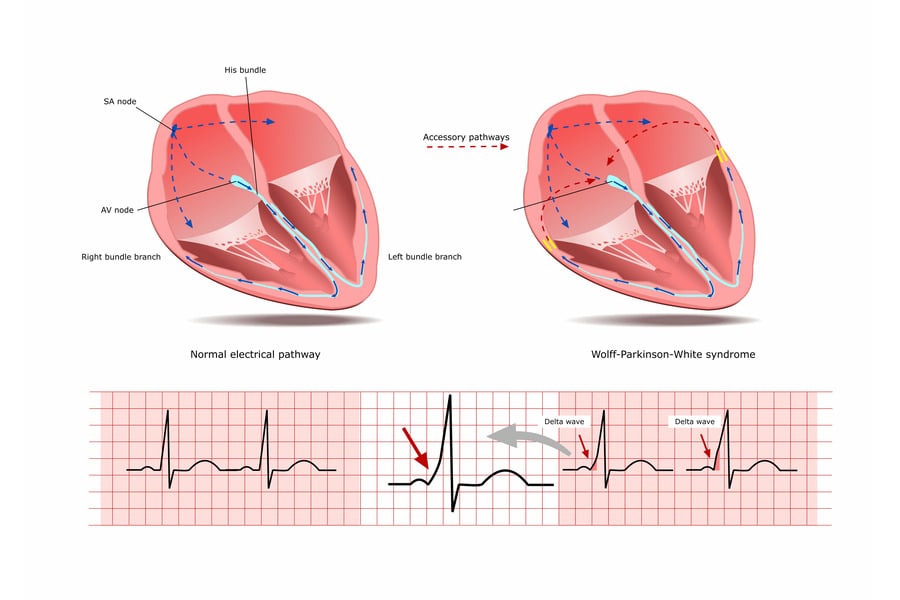
The heart’s electrical system controls the rhythm and rate of heartbeat. In WPW syndrome, the extra electrical pathway allows electrical signals to bypass the normal route, creating a loop of electrical activity. This can result in episodes of supraventricular tachycardia (SVT), a type of arrhythmia.
WPW syndrome can occur in people of all ages, including infants. Some individuals may experience symptoms, while others might not have any noticeable issues. For many, symptoms first appear during adolescence or young adulthood.
Symptoms
WPW syndrome may cause the following symptoms, especially during episodes of SVT:
- Palpitations or a rapid heartbeat
- Dizziness or lightheadedness
- Shortness of breath
- Fatigue
- Chest pain or discomfort
- Fainting (syncope)
It’s important to note that some individuals with WPW syndrome may not experience any symptoms.
Causes
WPW syndrome is a congenital condition, meaning it is present at birth. The exact cause of the extra electrical pathway is not known. However, it is believed to develop during the early stages of fetal heart development.
WPW syndrome can occur on its own or as part of a genetic syndrome, such as Ebstein’s anomaly or hypertrophic cardiomyopathy. In some cases, it may run in families, suggesting a genetic component.
Risk Factors
Risk factors for WPW syndrome may include:
- Family history of WPW syndrome or other arrhythmias
- Having a structural heart defect or other genetic syndromes
Prevention
Since WPW syndrome is a congenital condition, it cannot be prevented. However, individuals with WPW syndrome can take steps to reduce the risk of experiencing symptoms:
- Avoid triggers: Certain factors like alcohol, caffeine, stress, or lack of sleep can trigger SVT episodes.
- Manage other health conditions: Addressing related health issues like high blood pressure or thyroid problems can help reduce the risk of arrhythmias.
When to See a Doctor
Individuals who experience symptoms of WPW syndrome, such as palpitations or dizziness, should consult a healthcare professional. An electrocardiogram (ECG) can help diagnose WPW syndrome by revealing the extra electrical pathway.
Treatment and Management
Treatment for WPW syndrome focuses on preventing rapid heartbeats and managing symptoms. Options include:
- Medications: Antiarrhythmic drugs can help control heart rhythm.
- Vagal maneuvers: Techniques like coughing or bearing down can help slow down the heart rate during an episode of tachycardia.
- Cardioversion: Electric shocks can be used to restore a normal heart rhythm during an SVT episode.
- Catheter ablation: The extra electrical pathway can be destroyed using radiofrequency energy, often curing the condition.
- Lifestyle changes: Avoiding triggers and managing related health conditions can help reduce symptoms.
Additional Information:
WPW Pattern and WPW Syndrome
WPW pattern and WPW syndrome are two terms that are often used interchangeably but they represent different clinical entities. WPW pattern refers to the presence of the extra electrical pathway in the heart without any associated symptoms. WPW syndrome, on the other hand, is characterized by the presence of the extra pathway along with symptoms of arrhythmia.
Age of Onset
WPW syndrome can occur at any age, but it is most commonly diagnosed in children, teenagers, and young adults. Symptoms typically begin to appear between the ages of 11 and 50. Early diagnosis and appropriate management can help reduce the risk of complications associated with the condition.
Associated Conditions
WPW syndrome may be associated with other heart conditions such as Ebstein’s anomaly, a congenital heart defect that affects the tricuspid valve, or hypertrophic cardiomyopathy, a condition characterized by abnormal thickening of the heart muscle. These conditions may increase the risk of arrhythmias in individuals with WPW syndrome.
Prognosis
The prognosis for individuals with WPW syndrome is generally good. Many people with the condition do not experience any symptoms or complications. For those who do experience symptoms, treatment is usually effective at managing the condition. In rare cases, WPW syndrome may be associated with a risk of sudden cardiac arrest, particularly in individuals with a history of rapid heart rhythms.
Pre-Excitation
WPW syndrome is a type of pre-excitation syndrome. Pre-excitation refers to the early activation of a part of the heart due to the presence of an extra electrical pathway. In WPW syndrome, the extra pathway is known as the accessory pathway or bundle of Kent. The presence of this pathway can lead to the characteristic findings seen on an electrocardiogram (ECG), including a short PR interval and a delta wave.
In conclusion, Wolff-Parkinson-White Syndrome is a congenital heart condition that can lead to episodes of rapid heartbeats. The condition is caused by an extra electrical pathway in the heart. While it may cause symptoms like palpitations or dizziness, many individuals with WPW syndrome do not experience any issues. Treatment focuses on managing symptoms and preventing tachycardia episodes. By understanding the condition, individuals with WPW syndrome can effectively manage their heart health.