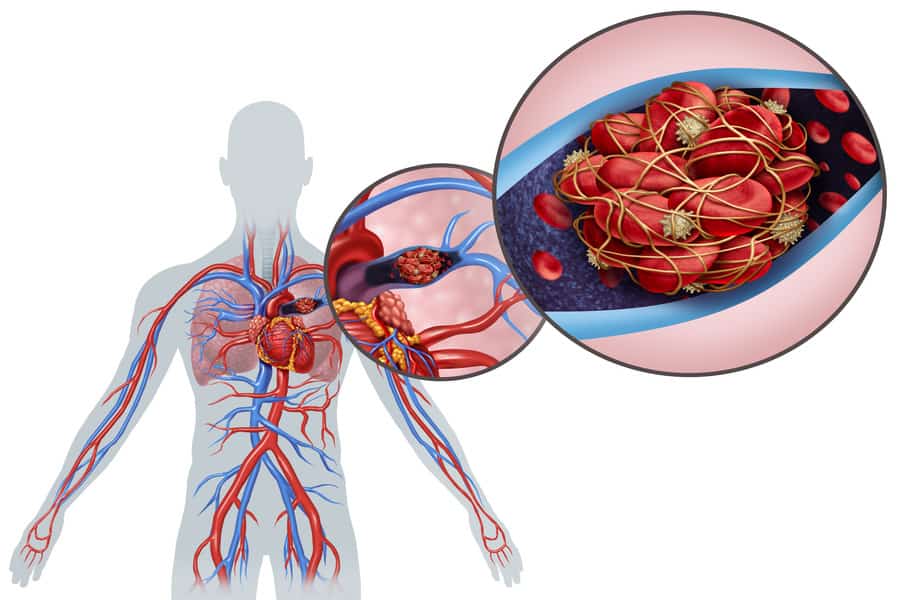
Pulmonary embolism (PE) is a potentially life-threatening medical condition characterized by the sudden blockage of a pulmonary artery in the lungs. This blockage usually occurs when a blood clot that formed elsewhere in the body, commonly in the legs or pelvis, travels through the bloodstream and becomes lodged in the lung artery.
Overview
Blood clots are necessary for stopping bleeding after an injury, but they can be problematic if they form when not needed or do not dissolve naturally. When a blood clot forms in a deep vein, usually in the legs, it is known as deep vein thrombosis (DVT). A piece of this clot can break off, travel through the bloodstream, and block a pulmonary artery, causing a pulmonary embolism.
PE can cause a wide range of symptoms, from mild to severe, and can be fatal if not promptly treated. The severity depends on the size of the clot, underlying health, and other factors.
Symptoms
Symptoms of pulmonary embolism may vary widely and can range from mild to severe, depending on factors such as the size of the clot and a person’s overall health. Common symptoms include:
- Shortness of breath: This symptom often appears suddenly and worsens with exertion.
- Chest pain: Can be sharp and may become more severe when you breathe deeply, cough, or eat. It may also radiate to the arm, shoulder, neck, or jaw.
- Cough: May produce bloody or blood-streaked sputum.
- Rapid heart rate: Tachycardia may occur.
- Sweating: Excessive sweating can occur.
- Fainting: Some people may faint due to low oxygen levels.
- Anxiety or uneasiness: Often accompanies this condition.
Causes
PE is usually caused by a blood clot that forms elsewhere in the body and then travels to the lungs. The main causes of these clots include:
- Deep vein thrombosis (DVT): Blood clots in the deep veins of the legs or pelvis, which can break off and travel to the lungs.
- Prolonged immobility: Long periods of inactivity, such as bed rest or long-haul flights, can cause blood to pool and clot.
- Surgery: Especially orthopedic surgeries, which can slow blood flow and increase clot risk.
Risk Factors
Several factors can increase the risk of PE:
- History of DVT or PE: Having had one of these conditions before.
- Surgery: Particularly surgeries that affect the pelvis, legs, abdomen, or brain.
- Long periods of immobility: Long-haul flights, bed rest, or being sedentary.
- Cancer: Certain types of cancer, and some treatments and surgeries for cancer.
- Smoking: Especially in combination with other risk factors.
- Pregnancy and childbirth: Especially during the first six weeks after childbirth.
Avoiding Pulmonary Embolism
Preventive measures include:
- Blood-thinners: Medications to prevent clots in high-risk individuals.
- Compression stockings: To prevent DVT in patients at risk.
- Regular movement: Moving the legs during long periods of immobility.
- Hydration: Staying well-hydrated helps prevent blood thickening.
- Healthy lifestyle: Regular exercise, balanced diet, and avoiding smoking.
When to See a Doctor
Immediate medical attention should be sought if you experience unexplained shortness of breath, chest pain, or a cough that produces bloody sputum.
Pulmonary Infarction:
Pulmonary embolism can lead to pulmonary infarction, a condition in which part of the lung tissue dies due to reduced blood flow. This condition can cause complications such as pneumonia and pleurisy (inflammation of the lining of the lungs and chest cavity).
Chronic Thromboembolic Pulmonary Hypertension (CTEPH):
In some cases, pulmonary embolism can lead to a condition called CTEPH, which is characterized by high blood pressure in the arteries of the lungs due to the buildup of old blood clots. This condition can cause symptoms such as shortness of breath, fatigue, and chest pain.
Diagnosis:
Pulmonary embolism can be diagnosed using a variety of tests, including chest X-rays, CT scans, pulmonary angiograms, and blood tests to detect elevated levels of clotting substances (D-dimer). Each test has its advantages and disadvantages, and the choice of test depends on factors such as the patient’s overall health and the severity of the symptoms.
Treatment Options:
The primary treatment for pulmonary embolism is anticoagulant medications, which help to prevent the formation of new blood clots and allow the body to dissolve existing clots. In some cases, clot-busting drugs (thrombolytics) may be used to dissolve large clots quickly. For patients who cannot take anticoagulants, an inferior vena cava (IVC) filter may be placed in the main vein leading to the heart to prevent clots from reaching the lungs.
In Conclusion, Pulmonary embolism is a serious condition that can be life-threatening without prompt treatment. Understanding the symptoms, risk factors, and prevention methods is key to reducing your risk and seeking timely help when needed. Managing the risk factors, including adopting a healthier lifestyle and avoiding prolonged immobility, can be a significant step in preventing this condition.