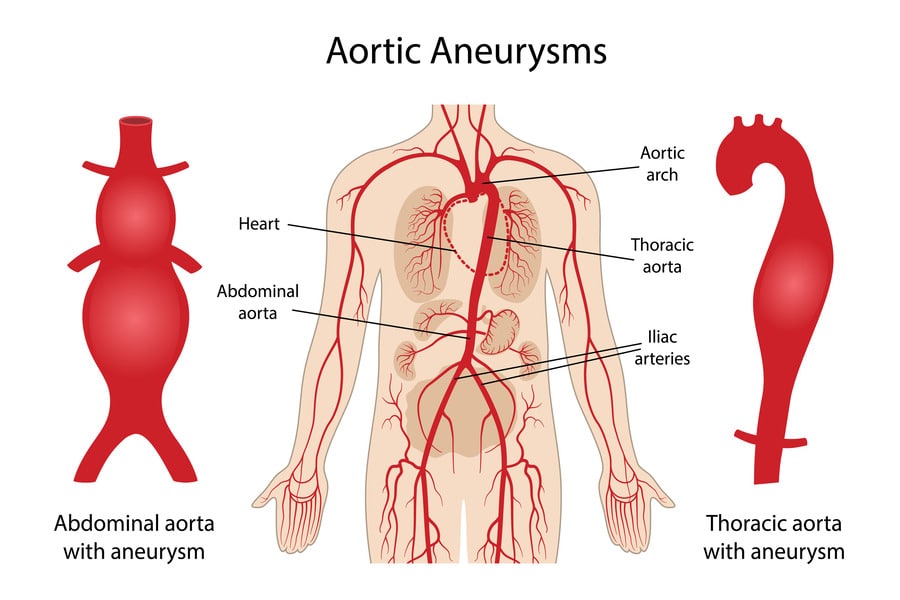
A thoracic aortic aneurysm is an abnormal bulging or widening of a portion of the aorta, the largest blood vessel in the body, as it passes through the chest (thoracic region). This condition can be life-threatening as the weakened area of the aorta is prone to rupture, causing severe internal bleeding.
Overview
The aorta is responsible for delivering oxygenated blood from the heart to the rest of the body. A thoracic aortic aneurysm occurs in the segment of the aorta that lies within the chest. This condition can go unnoticed as it often presents no symptoms until it becomes large or begins to leak blood or rupture.
Symptoms
Many thoracic aortic aneurysms do not cause any symptoms and are discovered incidentally during medical examinations for other reasons. However, if an aneurysm grows large, it may press on nearby structures and cause symptoms such as:
- Chest or back pain
- Shortness of breath
- Hoarseness
- Difficulty swallowing
- Coughing
In cases of rupture or dissection (a tear in the aorta’s wall), the symptoms can be sudden and severe, including:
- Sudden, sharp chest or back pain
- Loss of consciousness
- Difficulty breathing
Causes
Thoracic aortic aneurysms can be caused by a variety of factors, including:
- Aging: The risk increases with age, particularly after the age of 60.
- Atherosclerosis: Hardening and narrowing of the arteries due to plaque buildup.
- High blood pressure: Chronic hypertension can weaken the aortic wall.
- Genetic factors: Certain genetic conditions, such as Marfan syndrome, can increase the risk.
- Inflammation: Conditions like giant cell arteritis or Takayasu’s arteritis can cause inflammation of the aorta.
- Trauma: Injuries to the chest, such as those sustained in a car accident.
Risk Factors
Factors that increase the risk of developing a thoracic aortic aneurysm include:
- Smoking
- Family history of aortic aneurysm
- High cholesterol levels
- Obesity
- Male gender
Prevention
To reduce the risk of developing a thoracic aortic aneurysm or prevent its progression:
- Control blood pressure
- Quit smoking
- Maintain a healthy weight
- Exercise regularly
- Eat a balanced diet
- Manage cholesterol levels
When to See a Doctor
If you experience sudden, severe chest or back pain, seek emergency medical attention as it could be a sign of a ruptured aneurysm. If you have risk factors or a family history of aortic aneurysms, talk to your doctor about regular screenings.
Treatment
Treatment for thoracic aortic aneurysms depends on the size and growth rate of the aneurysm, as well as your overall health. Options include:
- Monitoring: Regular check-ups and imaging tests to monitor the aneurysm’s size and growth.
- Medications: Drugs to control blood pressure and reduce the risk of rupture.
- Surgery: If the aneurysm is large, growing rapidly, or causing symptoms, surgery may be recommended to repair or replace the affected section of the aorta.
Types of Thoracic Aortic Aneurysms
There are three types of thoracic aortic aneurysms:
- Ascending Aortic Aneurysm: This type occurs in the section of the aorta that ascends from the heart.
- Aortic Arch Aneurysm: This type occurs in the aortic arch, the curved section of the aorta that connects the ascending and descending aorta.
- Descending Aortic Aneurysm: This type occurs in the section of the aorta that descends through the chest.
Diagnosis
Thoracic aortic aneurysms are typically diagnosed using imaging tests, which can include:
- Chest X-ray: Can identify an enlarged aorta.
- Echocardiogram: Uses sound waves to produce images of the heart and aorta.
- CT Scan: Provides detailed images of the aorta, helping to determine the size and shape of the aneurysm.
- MRI: Creates images of the aorta using a magnetic field and radio waves.
Genetic Testing
If you have a family history of aortic aneurysms or certain genetic conditions that increase the risk (e.g., Marfan syndrome), your doctor may recommend genetic testing. Genetic counseling can provide information and support as you consider testing and interpret the results.
Lifestyle Management
In addition to the preventive measures mentioned in the article, the following lifestyle changes can further reduce the risk of thoracic aortic aneurysms:
- Limit alcohol consumption: Excessive alcohol intake can raise blood pressure and increase the risk of aneurysms.
- Reduce sodium intake: High sodium intake can contribute to high blood pressure.
- Manage stress: Chronic stress can contribute to high blood pressure.
Complications
If a thoracic aortic aneurysm ruptures or dissects, it can lead to life-threatening complications, including:
- Internal bleeding: A rupture can cause severe bleeding in the chest or abdomen, leading to shock and organ failure.
- Aortic dissection: A tear in the aortic wall can cause blood to flow between the layers of the vessel, leading to aortic rupture or reduced blood flow to vital organs.
Post-Surgery Care
After surgery to repair a thoracic aortic aneurysm, patients may need to take medications to manage blood pressure and cholesterol levels. Regular follow-up appointments and imaging tests are essential to monitor the repaired or replaced aorta and ensure there are no complications. Patients should discuss activity restrictions and rehabilitation with their healthcare team.
Thoracic aortic aneurysms are typically diagnosed using imaging tests, which can include:
- Chest X-ray: Can identify an enlarged aorta.
- Echocardiogram: Uses sound waves to produce images of the heart and aorta.
- CT Scan: Provides detailed images of the aorta, helping to determine the size and shape of the aneurysm.
- MRI: Creates images of the aorta using a magnetic field and radio waves.
Genetic Testing
If you have a family history of aortic aneurysms or certain genetic conditions that increase the risk (e.g., Marfan syndrome), your doctor may recommend genetic testing. Genetic counseling can provide information and support as you consider testing and interpreting the results.
Lifestyle Management
In addition to the preventive measures mentioned in the article, the following lifestyle changes can further reduce the risk of thoracic aortic aneurysms:
- Limit alcohol consumption: Excessive alcohol intake can raise blood pressure and increase the risk of aneurysms.
- Reduce sodium intake: High sodium intake can contribute to high blood pressure.
- Manage stress: Chronic stress can contribute to high blood pressure.
Complications
If a thoracic aortic aneurysm ruptures or dissects, it can lead to life-threatening complications, including:
- Internal bleeding: A rupture can cause severe bleeding in the chest or abdomen, leading to shock and organ failure.
- Aortic dissection: A tear in the aortic wall can cause blood to flow between the layers of the vessel, leading to aortic rupture or reduced blood flow to vital organs.
Post-Surgery Care
After surgery to repair a thoracic aortic aneurysm, patients may need to take medications to manage blood pressure and cholesterol levels. Regular follow-up appointments and imaging tests are essential to monitor the repaired or replaced aorta and ensure there are no complications. Patients should discuss activity restrictions and rehabilitation with their healthcare team.
In conclusion, thoracic aortic aneurysms can be life-threatening if they rupture, but many go unnoticed until they cause symptoms or are discovered incidentally. By understanding the risk factors and taking preventive measures, you can reduce your risk and improve your cardiovascular health. Regular check-ups and screenings are essential for early detection and appropriate management of thoracic aortic aneurysms.