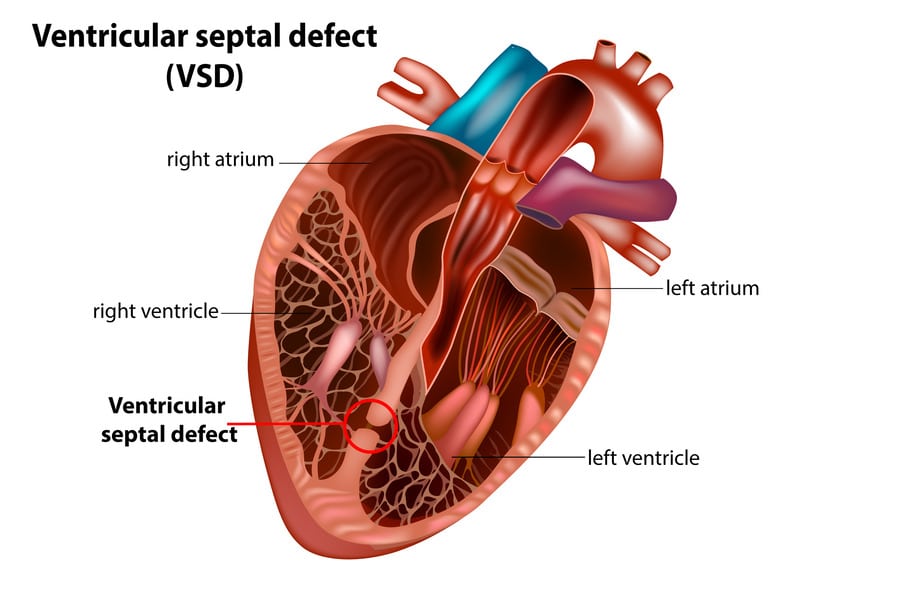
A ventricular septal defect (VSD) is a congenital heart condition characterized by a hole in the wall (septum) that separates the heart’s two lower chambers (ventricles). This hole allows oxygen-rich blood from the left ventricle to mix with oxygen-poor blood from the right ventricle, leading to inefficient blood circulation and putting additional strain on the heart.
Overview
VSD is one of the most common congenital heart defects, affecting approximately 2-6 out of every 1,000 newborns. While many VSDs are small and may close on their own during infancy or early childhood, some may require medical intervention or surgery, depending on the size and location of the defect.
Symptoms
VSD symptoms may vary depending on the size of the defect and the child’s age. In small VSDs, symptoms might be absent or mild, while large VSDs can cause more severe symptoms, such as:
- Rapid breathing or breathlessness
- Fatigue and weakness
- Poor weight gain and growth
- Frequent respiratory infections
- Cyanosis (bluish skin color)
- Heart murmur (an abnormal heart sound)
Causes
Ventricular septal defects occur during fetal heart development, usually within the first eight weeks of pregnancy. The exact cause is often unknown, but several factors may contribute to the development of VSD:
- Genetic factors: Family history of congenital heart defects increases the risk of VSD.
- Environmental factors: Exposure to certain chemicals or infections during pregnancy may increase the risk.
- Maternal conditions: Pre-existing conditions like diabetes, obesity, or poorly controlled blood pressure during pregnancy may contribute to the risk.
Risk Factors
Risk factors for VSD include:
- Family history of congenital heart defects
- Maternal exposure to certain medications or drugs during pregnancy
- Maternal medical conditions, such as diabetes or obesity
- Premature birth or low birth weight
Prevention
While some cases of VSD may be unavoidable, certain measures can reduce the risk:
- Prenatal care: Regular prenatal check-ups and screenings can help detect and manage potential risk factors.
- Avoid harmful substances: Pregnant women should avoid alcohol, tobacco, and illegal drugs.
- Medication management: Discuss the safety of medications with a healthcare provider during pregnancy.
- Manage pre-existing conditions: Properly managing diabetes, high blood pressure, and other medical conditions can reduce the risk.
When to See a Doctor
If your child exhibits symptoms of VSD, such as rapid breathing, fatigue, or poor weight gain, consult a pediatrician. A heart murmur may be an early sign of VSD and should be further evaluated by a pediatric cardiologist.
Treatment and Management
Treatment for VSD depends on the size, location, and symptoms of the defect:
- Observation: Small VSDs may close on their own and may only require regular monitoring.
- Medication: Diuretics, ACE inhibitors, or beta-blockers may be prescribed to manage symptoms and prevent complications.
- Cardiac catheterization: A device may be placed via catheterization to close the defect in some cases.
- Surgery: Large VSDs that cause significant symptoms or complications may require surgical repair.
Additional Information:
Follow-up Care
Follow-up care for VSD is crucial to monitor the progress of the defect, evaluate heart function, and manage any potential complications. Individuals with a history of VSD should continue regular check-ups with a cardiologist, even if the defect has closed or been repaired.
Potential Complications
Unrepaired or late-repaired VSDs may lead to complications:
- Pulmonary hypertension: Increased blood flow to the lungs can cause high blood pressure in the lung arteries, leading to respiratory problems and right-sided heart failure.
- Endocarditis: People with VSD are at a higher risk of developing bacterial endocarditis, an infection of the heart lining or valves.
- Arrhythmias: VSD can increase the risk of abnormal heart rhythms, affecting the heart’s ability to pump blood effectively.
- Heart failure: Over time, the increased workload on the heart can lead to heart failure.
Types of VSD
VSDs are classified based on their location within the ventricular septum:
- Membranous VSD: Located in the upper portion of the septum, near the aortic and tricuspid valves.
- Muscular VSD: Located in the lower, muscular portion of the septum.
- Inlet VSD: Located near the tricuspid valve.
- Outlet VSD: Located near the pulmonary valve.
Non-Surgical Closure of VSD
In some cases, VSDs can be closed without open-heart surgery. A device, often a small metal coil or mesh patch, is inserted through a catheter and guided to the defect to seal it. This minimally invasive approach is suitable for specific types of VSDs and offers faster recovery times.
In conclusion, Ventricular septal defect is a common congenital heart condition that may range from asymptomatic to severe. Proper prenatal care, early detection, and timely intervention are essential to prevent complications and ensure a healthy life for children with VSD. Consult with a pediatric cardiologist to determine the best approach for managing your child’s VSD.