Venous stasis, also known as venous stasis disease or stasis dermatitis, is a condition where the blood flow in the veins, particularly in the legs, slows down. This occurs when the vein valves become damaged or weak, leading to blood pooling in the veins, causing swelling, skin changes, and other symptoms. Venous stasis is a chronic condition and can lead to complications if left untreated.
Symptoms
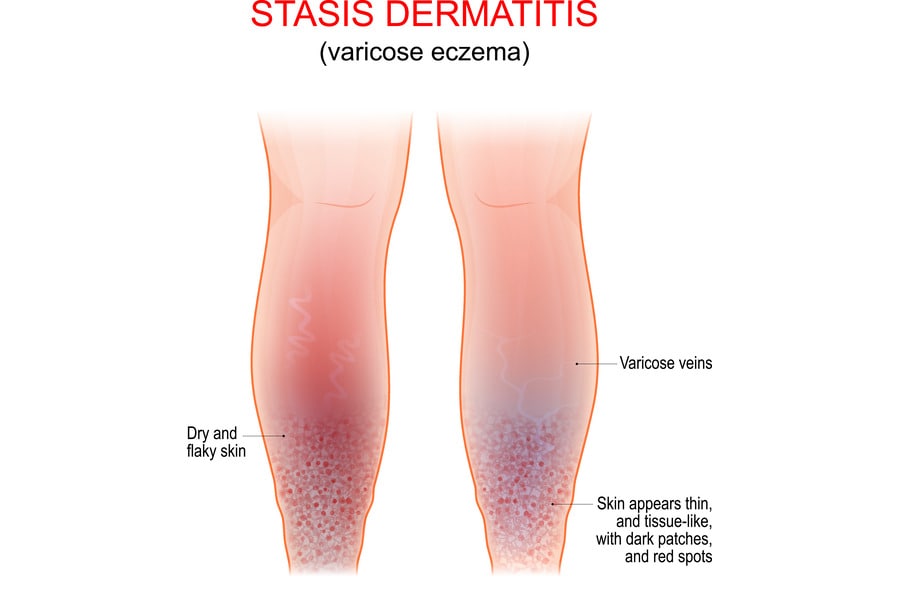
The symptoms of venous stasis can vary depending on the severity of the condition. Common symptoms include:
- Swelling in the legs or ankles
- Heaviness, aching, or pain in the legs
- Varicose veins
- Skin discoloration (darkening or reddening)
- Thickening or hardening of the skin
- Itchy or flaky skin
- Slow-healing sores or ulcers
Causes
Venous stasis typically results from damaged or weakened vein valves, which can be caused by:
- Aging: As people age, the valves in the veins can become less effective.
- Blood clots: A history of deep vein thrombosis (DVT) can damage vein valves.
- Varicose veins: These bulging veins can cause valve damage.
- Obesity: Excess weight puts pressure on the veins.
- Pregnancy: Increased blood volume during pregnancy can strain the veins and valves.
- Sedentary lifestyle: Sitting or standing for long periods can increase the risk.
Risk Factors
Several factors can increase the risk of developing venous stasis, including:
- Age: Older adults are more likely to develop this condition.
- Gender: Women are more prone to venous stasis, possibly due to hormonal changes.
- Obesity: Excess weight adds pressure to the veins.
- Pregnancy: The increased blood volume can strain the veins and valves.
- Family history: Genetics may play a role in the development of venous stasis.
- Sedentary lifestyle: Prolonged sitting or standing increases the risk.
Prevention
Preventing venous stasis involves taking measures to promote healthy blood flow, such as:
- Regular exercise: Physical activity encourages healthy blood circulation.
- Maintain a healthy weight: Reducing pressure on your veins helps prevent venous stasis.
- Avoid prolonged sitting or standing: Take breaks to move and stretch your legs.
- Wear compression stockings: These can help improve blood flow in the legs.
- Elevate your legs: Raising your legs above heart level helps reduce swelling.
When to See a Doctor
Seek medical help if you experience symptoms of venous stasis, like swelling, pain, or skin changes in your legs. Early diagnosis and treatment can help manage symptoms and prevent complications.
Diagnosis of Venous Stasis
Venous stasis diagnosis starts with a physical examination and a review of your medical history. Your doctor will ask about your symptoms, lifestyle, and any known risk factors. To confirm the diagnosis and assess the severity of venous stasis, your doctor may order imaging tests, such as:
- Duplex ultrasound: This non-invasive test uses sound waves to create images of the veins and assess blood flow, helping identify damaged valves or blood clots.
- Venogram: This is an X-ray of the veins, often performed with a contrast dye injection, to provide detailed images and help assess blood flow.
Treatment Options for Venous Stasis
The treatment for venous stasis aims to improve blood flow in the veins, relieve symptoms, and prevent complications. Treatment options may include:
- Lifestyle changes: Regular exercise, maintaining a healthy weight, and avoiding prolonged sitting or standing can help improve blood flow and reduce symptoms.
- Compression therapy: Wearing compression stockings can help reduce swelling and improve blood flow in the legs.
- Medications: Diuretics, pain relievers, and anti-inflammatory drugs can help manage symptoms. Topical treatments, like corticosteroids, can also help with skin-related symptoms.
- Minimally invasive procedures: Sclerotherapy, laser therapy, or radiofrequency ablation can be used to treat varicose veins and improve blood flow.
- Surgery: In severe cases, surgical options like vein stripping or valve repair may be necessary.
Complications of Venous Stasis
If left untreated, venous stasis can lead to complications, including:
- Varicose veins: These bulging, twisted veins can cause pain and discomfort.
- Venous ulcers: Slow-healing sores on the legs or ankles, often caused by poor blood flow.
- Cellulitis: A bacterial skin infection that can develop from venous ulcers.
- Deep vein thrombosis (DVT): A blood clot in a deeper vein, typically in the legs, which can cause pain and swelling and may lead to serious complications.
- Lipodermatosclerosis: A skin condition characterized by inflammation, hardening, and darkening of the skin on the legs.
In conclusion, Venous stasis is a chronic condition that affects blood flow in the veins, leading to various symptoms and complications. Understanding its causes, risk factors, and preventive measures is crucial for proper management. If you have risk factors for venous stasis or experience symptoms, consult a healthcare provider for proper assessment and treatment. Implementing lifestyle changes, following treatment recommendations, and taking proactive steps to protect your vein health can help prevent venous stasis and improve your overall cardiovascular health.