The Watchman procedure, a groundbreaking medical intervention, has revolutionized the way medical professionals treat atrial fibrillation (AFib) and reduce the risk of stroke. This article explores the significance of the Watchman procedure, its benefits, the procedure itself, patient eligibility, and its promising future in cardiovascular medicine.
Understanding Watchman:
AFib, a prevalent heart rhythm disorder, poses a significant risk of stroke. Irregular blood flow can cause blood clots to form in the heart’s left atrial appendage (LAA), increasing the likelihood of a clot escaping and causing a stroke. Medical professionals have long used anticoagulant medications, such as warfarin or direct oral anticoagulants (DOACs), as the primary approach to manage AFib and prevent stroke. However, some patients may find these medications intolerable, and there may be associated bleeding risks.
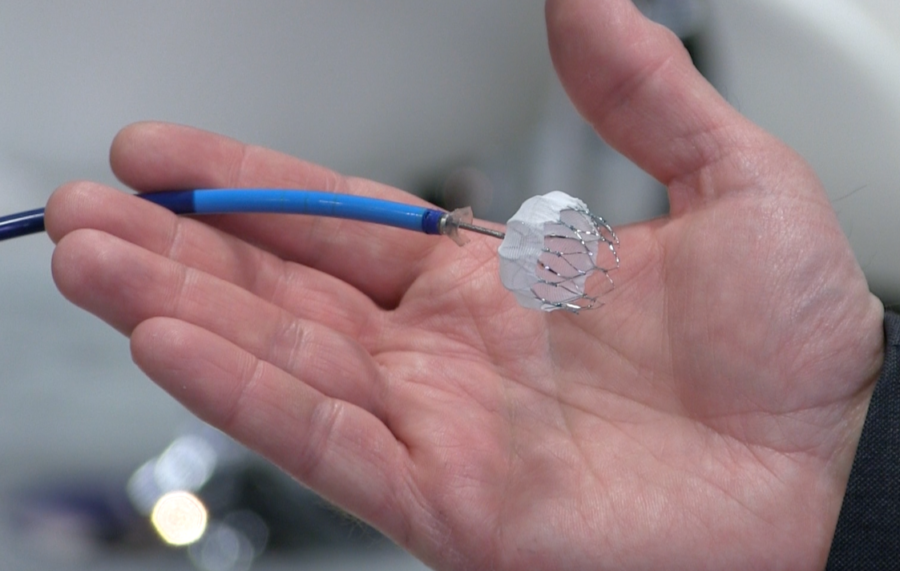
Enter the Watchman procedure – a transcatheter intervention that offers an alternative to long-term anticoagulant therapy. In this procedure, a small device is implanted into the LAA, sealing off this area and preventing the formation of blood clots.
The Benefits of Watchman:
The Watchman procedure offers several compelling advantages:
- Reduced Stroke Risk: By sealing off the LAA, the Watchman device significantly lowers the risk of stroke in AFib patients, providing them with peace of mind and improved quality of life.
- Alternative to Anticoagulants: The Watchman procedure is a viable option for patients who cannot tolerate or are ineligible for anticoagulant medications, offering a safe and effective stroke prevention alternative.
- Elimination of Long-Term Medication: Successful Watchman implantation may allow some patients to discontinue anticoagulant therapy, eliminating the need for daily medication and its associated side effects.
- Permanent Solution: The Watchman device remains in place indefinitely, providing lasting protection against stroke.
- Reduced Bleeding Risk: Unlike anticoagulants that carry the risk of bleeding, the Watchman procedure significantly reduces this risk, especially for patients prone to bleeding complications.
The Watchman Procedure:
Healthcare professionals, including interventional cardiologists and electrophysiologists, perform the Watchman procedure in a specialized cardiac catheterization laboratory. The steps involved in the procedure are as follows:
Pre-Procedure Preparations:
Before the Watchman procedure, healthcare professionals conduct comprehensive evaluations, including imaging tests such as transesophageal echocardiography (TEE) or cardiac computed tomography (CT). These tests help determine the LAA’s size and anatomy, guiding the selection of the appropriate Watchman device size.
- Anesthesia and Incision: During the procedure, patients receive general anesthesia to ensure comfort and immobility. The procedure commences with a small incision in the upper leg or groin area, providing access to the blood vessels.
- Catheter Insertion: A catheter is threaded through the blood vessels and advanced to the heart. Using fluoroscopy and contrast dye, healthcare professionals navigate the catheter to the LAA.
- Watchman Device Placement: The Watchman device, resembling a small parachute made of pliable materials, is carefully placed within the LAA. The device’s design allows it to conform to the LAA’s shape, effectively closing off the area to prevent blood clot formation.
- Confirmation and Closure: Once the Watchman device is in place, its position and sealing ability are confirmed through imaging tests, typically a TEE. After confirmation, healthcare professionals remove the catheter and close the incision site.
- Recovery and Follow-Up: Patients usually stay in the hospital overnight for observation after the Watchman implantation. Subsequently, regular follow-up visits are scheduled to ensure the device’s efficacy and monitor for any potential complications.
- Patient Eligibility: While the Watchman procedure offers a promising solution for stroke prevention in AFib patients, not all individuals are eligible candidates. Patient eligibility is determined through careful assessment, considering various factors such as LAA size, anatomy, overall health, and the ability to tolerate antiplatelet medications. Patients with a high bleeding risk or significant structural heart conditions may not be suitable candidates for the Watchman procedure
The Future of Watchman:
The Watchman procedure has rapidly gained popularity since regulatory authorities approved it. As medical technology advances, we can expect further refinements and improvements to the procedure. Ongoing research aims to explore its application in broader patient populations and refine implantation techniques. Additionally, long-term studies are evaluating the device’s durability and efficacy in preventing stroke over extended periods.
In suWatchman procedure represents a significant advancement in cardiovascular medicine, offering an innovative approach to reducing the risk of stroke in patients with AFib. As an alternative to long-term anticoagulant therapy, it provides patients with greater flexibility and reduces the risk of bleeding complications. The Watchman procedure’s success lies in its ability to close off the LAA, preventing the formation of blood clots and lowering the risk of stroke in AFib patients.
With its compelling benefits and ongoing research efforts, the Watchman procedure promises to continue transforming stroke prevention in AFib patients. As medical professionals and researchers strive to enhance patient outcomes and improve the procedure’s efficacy, the future holds great promise for the Watchman device as an essential tool in the fight against stroke in individuals living with AFib. As technology and medical knowledge advance hand in hand, the Watchman procedure stands as a beacon of hope for improved cardiovascular health and a safer, more sustainable approach to stroke prevention in the realm of modern cardiology.